Navigating the 2025 Medicare Fee Schedule: What Providers and Patients Need to Know
The Centers for Medicare & Medicaid Services (CMS) releases the Medicare Fee Schedule annually, outlining payment policies and rates for healthcare services provided to Medicare beneficiaries. Understanding the nuances of the 2025 Medicare Fee Schedule is crucial for healthcare providers to ensure accurate billing and revenue cycle management, and for patients to anticipate potential out-of-pocket costs. This article will delve into the key aspects of the upcoming fee schedule, providing a comprehensive overview of anticipated changes and their implications.
Understanding the Medicare Fee Schedule
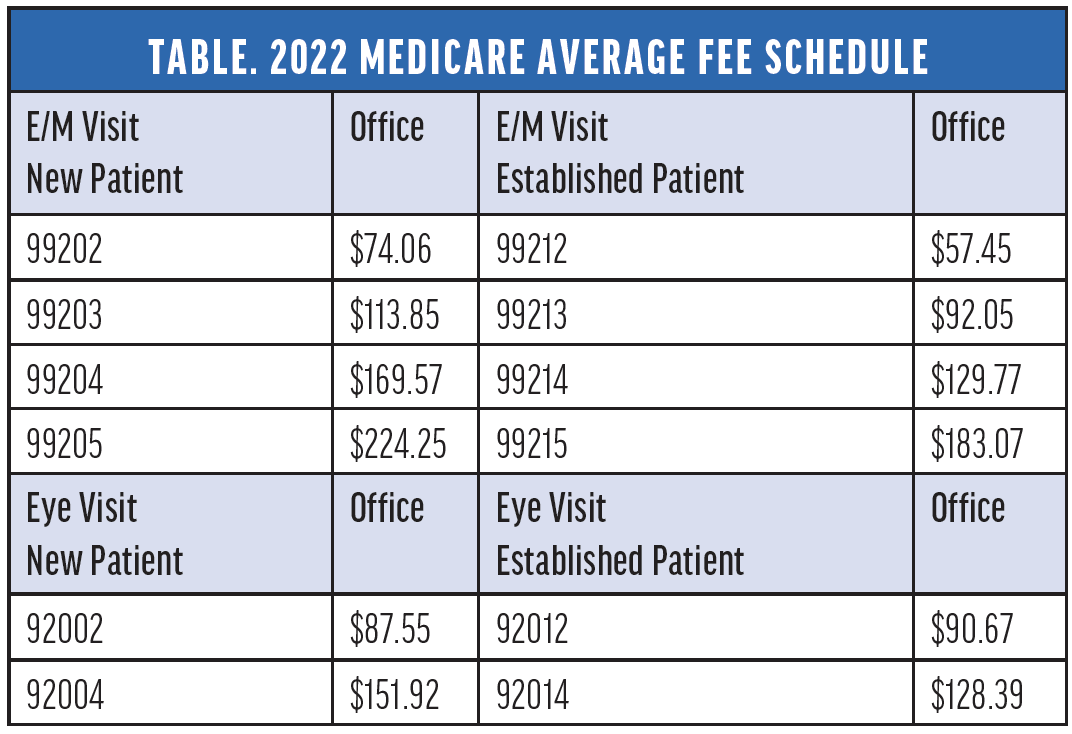
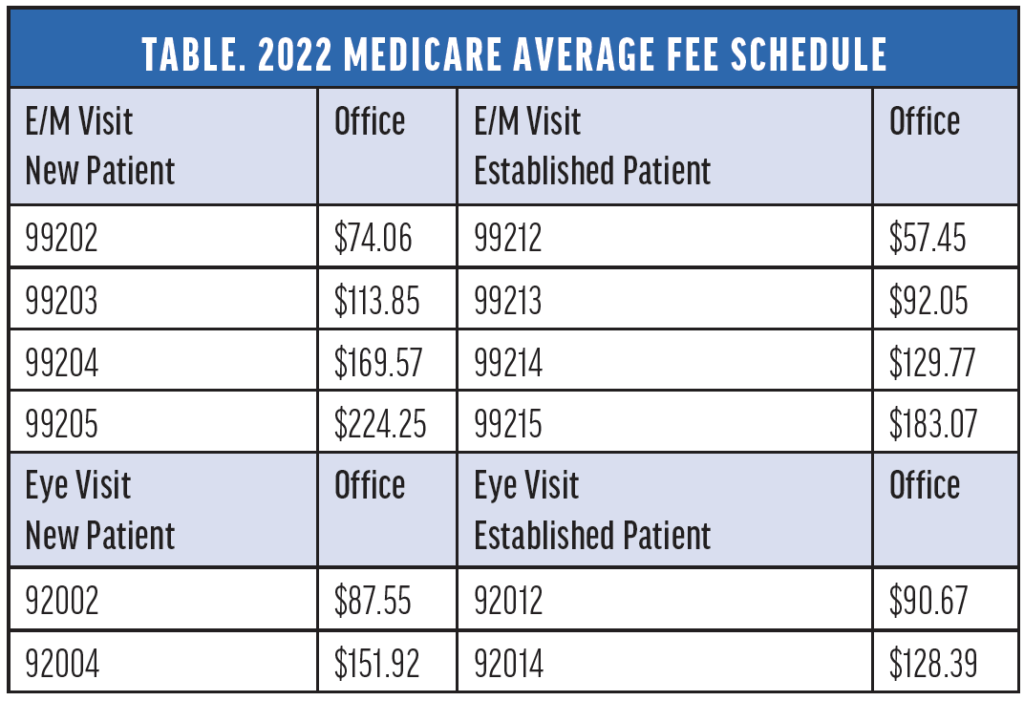
The Medicare Fee Schedule is a comprehensive list of fees used by Medicare to pay doctors, hospitals, and other healthcare providers. It’s based on a resource-based relative value scale (RBRVS), which considers the resources required to provide a service, including physician work, practice expense, and malpractice insurance. Each service is assigned a relative value unit (RVU), which is then multiplied by a conversion factor to determine the payment amount.
The conversion factor is updated annually and can significantly impact reimbursement rates. Changes to the 2025 Medicare Fee Schedule conversion factor are always closely watched by the healthcare industry. Beyond the conversion factor, the fee schedule also includes updates to coding guidelines, coverage policies, and other regulatory changes that can affect how services are billed and reimbursed.
Key Areas of Focus for the 2025 Medicare Fee Schedule
While the final details of the 2025 Medicare Fee Schedule are still being finalized, several key areas are likely to be focal points. These include:
Telehealth Services
The expansion of telehealth services during the COVID-19 pandemic led to temporary waivers and flexibilities in Medicare coverage. As the public health emergency ends, CMS is evaluating which telehealth services should be permanently included in the Medicare program. The 2025 Medicare Fee Schedule is expected to address the long-term coverage and payment policies for telehealth, including originating site requirements, audio-only services, and the use of technology-assisted care.
Evaluation and Management (E/M) Coding
Recent updates to E/M coding guidelines have simplified the process for selecting the appropriate level of service. The 2025 Medicare Fee Schedule will likely continue to refine these guidelines and address any implementation challenges. Providers should pay close attention to changes in documentation requirements and billing practices for E/M services.
Chronic Care Management (CCM)
CCM services are designed to improve the health outcomes of patients with chronic conditions. The 2025 Medicare Fee Schedule may include changes to the payment rates and eligibility requirements for CCM services. CMS is also exploring ways to expand access to CCM and integrate it with other care management programs.
Behavioral Health Services
Addressing the nation’s mental health crisis is a priority for CMS. The 2025 Medicare Fee Schedule could include initiatives to increase access to behavioral health services, such as expanding coverage for mental health counseling, substance use disorder treatment, and integrated care models. Increased reimbursement rates for certain behavioral health services may also be considered.
Value-Based Care Initiatives
CMS is committed to transitioning the healthcare system towards value-based care, which rewards providers for delivering high-quality, cost-effective care. The 2025 Medicare Fee Schedule may include updates to existing value-based care programs, such as the Medicare Shared Savings Program (MSSP) and the Quality Payment Program (QPP). New models of care delivery and payment may also be introduced to promote better outcomes and reduce healthcare costs.
Potential Impact on Providers
The 2025 Medicare Fee Schedule will have a significant impact on healthcare providers. Changes to reimbursement rates can affect revenue streams and profitability. It is crucial for providers to carefully analyze the fee schedule and understand how it will affect their specific services and patient populations.
Here are some potential impacts:
- Revenue Adjustments: Changes to the conversion factor and RVUs can lead to increases or decreases in reimbursement for specific services.
- Coding and Billing Compliance: Updated coding guidelines and coverage policies require providers to stay informed and ensure accurate billing practices.
- Investment in Technology: Expanding telehealth services and value-based care initiatives may require providers to invest in new technologies and infrastructure.
- Administrative Burden: Navigating the complexities of the fee schedule and implementing necessary changes can increase administrative burden for providers.
Potential Impact on Patients
The 2025 Medicare Fee Schedule also has implications for Medicare beneficiaries. Changes to coverage policies and cost-sharing requirements can affect patients’ access to care and out-of-pocket expenses.
Here are some potential impacts:
- Access to Telehealth: The expansion or contraction of telehealth services can impact patients’ ability to access care remotely.
- Cost-Sharing Requirements: Changes to deductibles, co-pays, and coinsurance can affect patients’ out-of-pocket costs for healthcare services.
- Coverage for New Services: The addition of new services to the Medicare program can expand patients’ access to innovative treatments and technologies.
- Impact of Value-Based Care: Value-based care initiatives can improve the quality of care and patient outcomes, but they may also require patients to actively participate in their own health management.
Strategies for Providers to Prepare
To prepare for the 2025 Medicare Fee Schedule, providers should take the following steps:
- Review the Proposed Rule: CMS typically releases a proposed rule for the Medicare Fee Schedule in the summer. Providers should carefully review the proposed rule and submit comments to CMS.
- Analyze the Final Rule: Once the final rule is released, providers should conduct a thorough analysis to understand the specific changes that will affect their practice.
- Update Coding and Billing Practices: Providers should update their coding and billing practices to reflect the new guidelines and coverage policies.
- Train Staff: It is important to train staff on the changes to the fee schedule and ensure they understand the new requirements.
- Monitor Reimbursement Rates: Providers should monitor their reimbursement rates to ensure they are being paid correctly.
- Invest in Technology: Providers should consider investing in technology to support telehealth services and value-based care initiatives.
- Engage with Professional Organizations: Professional organizations can provide valuable resources and advocacy on behalf of providers.
Resources for Staying Informed
Staying informed about the 2025 Medicare Fee Schedule is essential for both providers and patients. Here are some resources to help you stay up-to-date:
- Centers for Medicare & Medicaid Services (CMS): The CMS website (cms.gov) is the primary source of information about the Medicare Fee Schedule.
- Professional Organizations: Professional organizations, such as the American Medical Association (AMA) and the American Academy of Family Physicians (AAFP), provide updates and analysis of the fee schedule.
- Healthcare News Outlets: Healthcare news outlets, such as Modern Healthcare and Becker’s Hospital Review, provide coverage of the Medicare Fee Schedule and other healthcare policy issues.
- Consulting Firms: Healthcare consulting firms can provide expert guidance on navigating the complexities of the fee schedule.
Conclusion
The 2025 Medicare Fee Schedule will bring significant changes to the healthcare landscape. By understanding the key areas of focus and taking proactive steps to prepare, providers can mitigate the potential impact on their revenue and ensure they are providing high-quality care to their patients. Patients should also stay informed about the changes to the fee schedule to understand how it may affect their access to care and out-of-pocket expenses. Keeping abreast of updates to the 2025 Medicare Fee Schedule is crucial for all stakeholders in the healthcare ecosystem. Proactive preparation and a thorough understanding of the 2025 Medicare Fee Schedule are essential for navigating the evolving healthcare landscape. The implications of the 2025 Medicare Fee Schedule extend beyond financial considerations, influencing patient care and access to services. The 2025 Medicare Fee Schedule will shape the future of healthcare delivery in the United States. Staying informed about the 2025 Medicare Fee Schedule is a continuous process that requires ongoing monitoring and analysis. The 2025 Medicare Fee Schedule will be a topic of discussion and debate throughout the year. The complexities of the 2025 Medicare Fee Schedule require careful attention to detail. The 2025 Medicare Fee Schedule is a critical component of the U.S. healthcare system. Understanding the 2025 Medicare Fee Schedule is essential for all stakeholders. Changes to the 2025 Medicare Fee Schedule can have a ripple effect throughout the healthcare industry. A comprehensive understanding of the 2025 Medicare Fee Schedule allows for informed decision-making. The 2025 Medicare Fee Schedule is a reflection of the evolving healthcare landscape.
[See also: Understanding Medicare Advantage Plans]
[See also: The Future of Telehealth Reimbursement]
[See also: Navigating Healthcare Reform]